Does Gluten Sensitivity Exist?
By Calvin Sun
A recent video going around the Internet has highlighted that many people choosing to go on gluten-free diets have no idea what gluten is or why they are avoiding it. There seems to be some confusion regarding celiac disease (CD), gluten sensitivity in non-celiacs, and gluten itself. Gluten-free options have become widely available in recent years. This can range from a variety of gluten-free products at the grocery store to restaurants that have entire menus that are built around being gluten-free. People who suffer from CD have to avoid gluten at all costs but does gluten intolerance exist in non-celiacs?
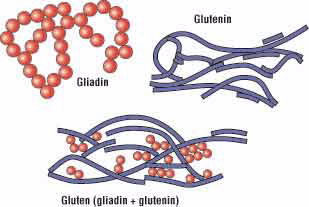
What Is Gluten?
Gluten is a protein composite made of two proteins: gliadin and glutenin. Gluten is most commonly found in wheat products but it’s also found in other cereal grains like barley, rye, and spelt. The protein composite allows for dough to be elastic and it helps create the chewy texture and structure of foods like bread and pasta. Gluten is also frequently used as a stabilizer, emulsifier, and thickening agent in many sauces, dressings, and condiments.
Does Gluten Cause Celiac Disease?
Gluten has been associated with a variety of health problems including gastrointestinal issues as well as autoimmune disorders. CD is probably the condition most commonly associated with gluten-free diets.
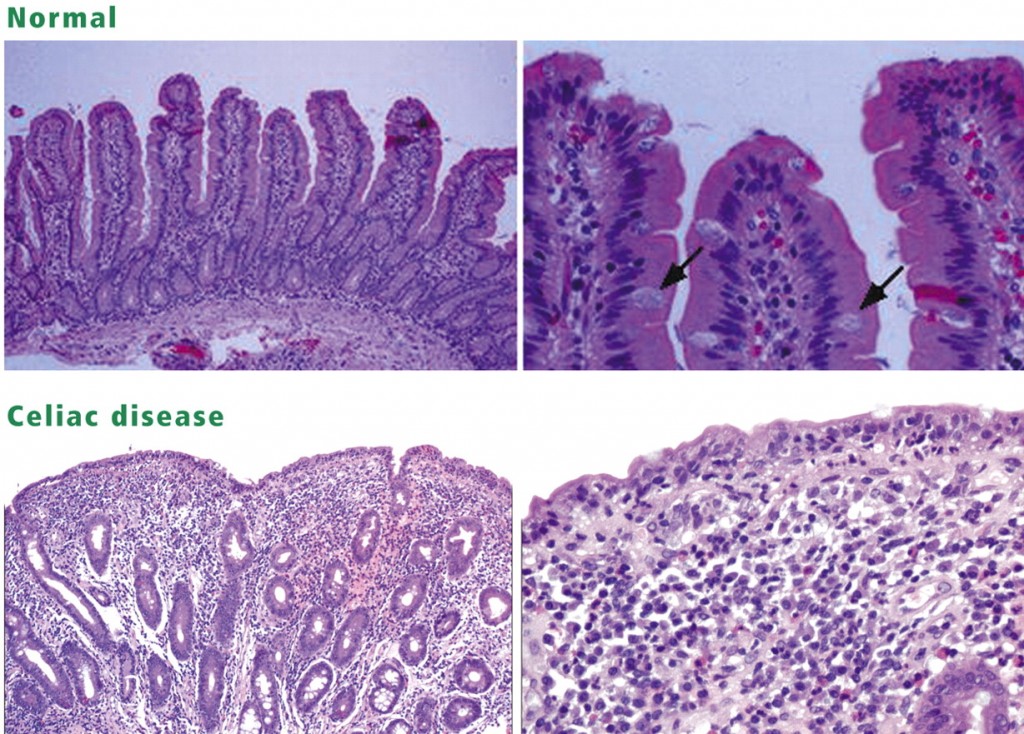
CD is an autoimmune disorder that results in severe inflammatory reactions in the small intestine when gluten, specifically gliadin, is present. This inflammatory response causes the microvilli in the intestinal lining to atrophy resulting in a decreased ability to absorb nutrients. It can also affect the permeability of the gut lining which can allow a variety of substances to pass into the bloodstream and cause other problems throughout the body. If untreated, people with CD can suffer from a range of problems including malnutrition, diarrhea, fatigue, abdominal cramping, neurological illnesses, and immune dysfunctions.
According to the American Journal of Gastroenterology, CD affects 1 in 141 people in the United States, which is about 0.7% of the population. Gluten consumption by itself doesn’t cause CD, as it is usually the result of a combination of genetic and environmental factors. Currently, the only effective treatment for those with CD is a strict gluten-free diet [1,3]. If you believe you may have CD, it’s advisable to see a gastroenterologist for a proper diagnosis. Testing usually includes blood tests for gluten antibodies and a biopsy of your small intestine to assess gut damage.
What is Non-Celiac Gluten Sensitivity (NCGS)?
Given the relatively low incidence of CD and the massive commercial market for gluten-free products, it’s probably safe to say the majority of people on gluten-free diets are non-celiacs. Many people report that they feel better on a gluten-free diet despite being a non-celiac. Generally speaking, non-celiacs report improvements in their health ranging from reduced gastrointestinal symptoms, reduced joint inflammation, improved skin complexion, and increased mental clarity.
However, some new research suggests that gluten intolerance in non-celiacs might not exist. The research suggests that this may just be a placebo effect. You can read the full text online.
If you don’t feel like reading the full study, I’ll give a brief summary of their experiment. Researchers had a group of non-celiac patients with gluten sensitivity and IBS eat a reduced FODMAP diet (see below) for 2 weeks and then placed them on a high-gluten, low-gluten, or gluten-free control diet for 1 week. After a washout period, participants were then crossed over to one of the other groups for 3 days. They found that all participants experienced improved gastrointestinal symptoms during the low-FODMAP period, but their symptoms worsened with high-gluten, low-gluten, and the gluten-free control [10]. The implication is that FODMAPs may play a larger role in gastrointestinal symptoms than gluten in those with NCGS. Researchers found that over 90% of NCGS patients did NOT experience gluten-specific reactions.
While there may some degree of a nocebo effect, this study doesn’t disprove the existence of NCGS. Another recent study in the Journal of Clinical Gastroenterology compared biomakers and levels of gluten-specific antibodies between NCGS patients and CD patients. Both groups were found to have elevated levels of anti-gliadin antibodies (AGA). Over half of the NCGS patients tested positive for AGA and over 80% of CD patients also tested positive [4]. Based on these results, it would appear that NCGS does exist. These elevated levels of AGA suggest that some cases of NCGS could be the result of an allergy.
This could mean that gluten-free works for some because they are gluten-intolerant and may work for others because of the reduction in FODMAP consumption. Either way, it appears that it can be an effective dietary strategy for reducing GI related issues.
What Is a FODMAP?
FODMAP is an acronym that stands for “Fermentable, Oligo-, Di-, Mono-saccharides And Polyols”. These are a class of carbohydrates and related alcohols that are poorly digested and can exacerbate gut symptoms [8]. FODMAPs not absorbed in the small intestine will pass into the large intestine. Once in the large intestine, bacterial fermentation and increased fluid movement can result in gas, pain, bloating, and diarrhea [9].
Wheat, rye, and barley are common sources of FODMAPs. As a result, bread products tend to be a rich source of FODMAPs in many modern diets. This might explain why going gluten-free helps improve symptoms in many people. And this might also explain why some people still have GI symptoms despite eating lots of gluten-free products.
Should I Go Gluten-Free?
If you think you might have a gluten intolerance, consider going 30 days with no gluten and minimal intake of FODMAPs. Make note of any differences you feel in your GI health, athletic performance, and mental clarity. At the end of 30 days, reintroduce gluten and see if it causes a reaction. If your symptoms improved during the 30 day period and worsened with the reintroduction of gluten, it’s possible that you have NCGS. If your symptoms improved during the elimination period, but did not return with reintroduction of gluten, it’s possible that you have a FODMAP intolerance. If you continue to have issues despite reducing FODMAPs and gluten, it’s advisable to consult with a medical professional.
References
1. Di Sabatino A, Corazza GR. Coeliac disease. Lancet. 2009 Apr 25;373(9673):1480-93.
2. Alberto Rubio-Tapia MD, Jonas F Ludvigsson MD, PhD, Tricia L Brantner, Joseph A Murray MD, and James E Everhart MD, MPH. The Prevalence of Celiac Disease in the United States. Am J Gastroenterol 2012; 107:1538–1544; doi:10.1038/ajg.2012.219; published online 31 July 2012
3. Kupper C. Dietary guidelines and implementation for celiac disease. Gastroenterology. 2005 Apr;128(4 Suppl 1):S121-7.
4. Volta, Umberto MD; Tovoli, Francesco MD; Cicola, Ronny MD; Parisi, Claudia MD; Fabbri, Angela MD; Piscaglia, Maria MD; Fiorini, Erica MD; Caio, Giacomo MD. Serological Tests in Gluten Sensitivity (Nonceliac Gluten Intolerance). Journal of Clinical Gastroenterology: September 2012 – Volume 46 – Issue 8 – p 680–685.
5. Maria Teresa Bardella, Clara Fredella, Valeria Saladino, Cristina Trovato, Bruno Mario Cesana, Maurizio Quatrini and Luigia Prampolini. Gluten intolerance: Gender- and age-related differences in symptoms. 2005, Vol. 40, No. 1, Pages 15-19.
6. Sapone et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Medicine 2011, 9:23.
7. Biesiekierski JR, Newnham ED, Shepherd SJ, Muir JG, Gibson PR. Characterization of Adults With a Self-Diagnosis of Nonceliac Gluten Sensitivity. Nutr Clin Pract. 2014 Apr 16.
8. Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252-8.
9. Jacqueline S. Barrett. Fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) and nonallergic food intolerance: FODMAPs or food chemicals?. Therapeutic Advances in Gastroenterology July 2012 vol. 5 no. 4 261-268.
10. Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013 Aug;145(2):320-8.e1-3.
I’m happy to see a continued discussion of nutrition topics on the blog. I tend to read them intently. That said, you have to be careful with statements like this one: “While there may some degree of a nocebo effect, this study [7] doesn’t disprove the existence of NCGS.” No single study can ever prove / disprove the existence of a condition, in this case NCGS. That’s not how the scientific method works. This study does provide very strong evidence that gluten is not a primary effect of what is termed NCGS, given the study design and the sample size… Read more »