
Patellar Pain – Are We Properly Addressing the Issue?
Written by Michele Vieux
Do you suffer from persistent knee pain? Done physical therapy with limited results? Changed your training routine or life because of your pain? Well you are not alone.
Patellofemoral pain syndrome (PFPS) is one of the most common conditions limiting athletes. PFPS is often used as an umbrella term for abnormal patella tracking due to: decreased flexibility of the quadriceps, hamstrings, iliotibial band, and gastrocnemius; decreased strength of the quadriceps and hamstrings; joint laxity; deviations in patellar mobility and tilting; and increased quadriceps angle.
Often times, people complain of pain around their kneecap that may limit their ability to perform activities of daily living that require loading on a flexed knee. Such activities include descending stairs, squatting, and sitting for prolonged periods of time.
How PFPS is Currently Treated
If you’ve experienced treatment for PFPS in the past, it is likely that your work has focused on addressing the symptoms i.e. the reasons for abnormal patella tracking and not the actual issue itself. It’s kind of like just wiping the blood away from a wound but not actually doing anything to stop the bleeding.
That’s because current therapy for PFPS focuses on addressing factors in the injured athlete, assuming that they are causes and not symptoms. Treatments you might have tried include vastus medialis oblique (VMO) retraining, open kinetic chain and isokinetic strengthening, patellar realignment orthoses, patellar mobilization, sacroiliac manipulation, low-level laser, acupuncture, and patellar taping all of which address the aforementioned conditions.
But is it possible that if these tools are only addressing the symptoms, there might be another reason or cause for development of PFPS that can be addressed to actually fix the problem instead of just bandage it?
A New Intervention Strategy for PFPS
A systematic review evaluated popular treatments and they found little evidence in support of the above interventions, as you may have experienced yourself. Pain reduction across all interventions was short-term, at best and no more effective than a home-based exercise program. (Crossley) However there is a growing body of evidence suggesting that dysfunction at the hip may be a contributing factor in PFPS. (Meira) That’s right, the cause could be in an area outside of the knee itself!
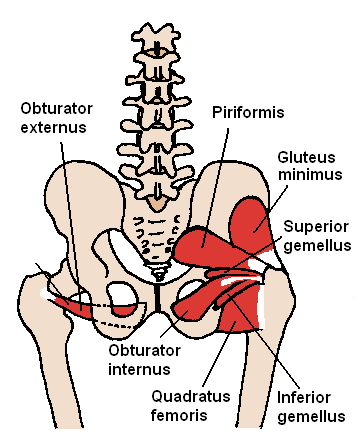
PFPS is associated with decreased hip strength, specifically at the abductors and external rotators. The lateral rotator group is a group of six small muscles of the hip which all externally (laterally) rotate the femur in the hip joint. It consists of the following muscles: Piriformis, gemellus superior, obturator internus, gemellus inferior, quadratus femoris and the obturator externus. All muscles in the lateral rotator group originate from the hip bone and insert on to the upper extremity of the femur. (See illustration below)
Since the hip abductors – and the commonly overlooked ROTATORS – can affect knee valgus, increasing rotation strength (both external and internal) may help athletes with PFPS. There is a correlation between PFPS and faulty hip mechanics (adduction and internal rotation). (Meira)
Working it into Your Routine
Assuming you don’t have someone to help you with your exercises, here are three simple rotator exercises you can add into your warm-up routine. As we talk about rotation of the hip, it is important to note the difference between rotation and adduction/abduction. With adduction/abduction, your legs will be moving laterally like scissors. With rotation, the head of the femur will rotate in a partial circle within the hip capsule like when you use a hand-held lemon juicer.
(above) Side-Lying Hip Rotations (3 positions) x 20 reps per position. Lay on one side and elevate your leg so that it is parallel to the floor in one of the three positions (legs stacked; top leg slightly forward; top leg slightly behind). Your foot should be hanging off whatever you use to elevate it so that it has room to rotate. Using ONLY your rotator muscles, internally and externally rotate your hip 20 reps. Since we are so used to activating our quads, hamstrings and glutes, you will find that it is extremely difficult at first to isolate those tiny muscles but when you do, you’ll know it! It is possible that you might not be able to control the rotation one direction or the other at first. In that case, do “negatives” like we do with pull-ups meaning, resist the urge to let your hip snap back into place but instead, guide it there. Just a note, the movement you see will be very small, like only an inch in each (circular) direction.
(above) Once the side-lying rotations are easy, start using those as a warm-up to this standing version. Standing Hip Rotations x 20 per leg. Stand with your feet side-by-side at hip width. Applying about 10-50% of your bodyweight to the leg you are working, perform your internal and external rotations. Again, the movement will be very small.
(above) Once the standing version is easy, replace it with this Banded Hip Rotation upgrade. Continue to do the side-lying rotations as a warm-up. Then hook up a light resistance band to a post at knee height. Stand next to the post laterally and step into the band facing either direction. Place the band, with tension, across the center of the kneecap. Perform your hip rotations against the resistance of the band. Turn and face the other direction and repeat. When the band is crossed over your body, you are performing external rotations.
Are We Properly Addressing the Issue?
Historically, PFPS has been viewed exclusively as a knee problem but recent findings have suggested an association between hip muscle weakness and PFPS. So which is it? Well that’s the the big question because if we can determine that, then we can treat the cause instead of the symptom. If you’ve been trying the traditional treatment with limited, temporary or no success, it might be time to get those hip rotators involved. Let us know what has helped with your knee pain in the comments!
Article Sources:
Bolgla et al. Comparison of Hip and Knee Strength and Neuromuscular Activity in Subjects with and without Patellofemoral Pain Syndrome. Int J Sports Phys Ther. 2011 Dec; 6(4): 285–296.
Crossley K, Bennell K, Green S, McConnell J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med. 2001;11:103-110
Meira, Erik P. Influence of the Hip on Patients With Patellofemoral Pain Syndrome. Sports Health. 2011 Sep; 3(5): 455–465.
Also Check Out…
4 Reasons You Struggle With Toes To Bar
I am going to try this out. I post comments after I understand the movements and utilize for a month. Thank you for a great article.